Introduction
The term hip is often used by people to describe a region that is actually part of their buttock. Pain in that region may be from the lower back, pelvis, soft tissues in the buttock and also from the hip joint itself. An important aim of the full history and examination is to determine where the problem is located.
Anatomy of the Hip
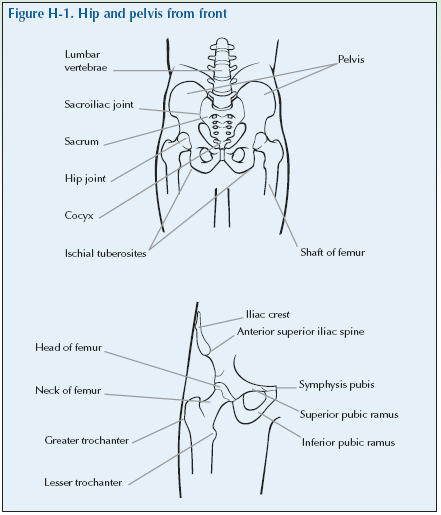
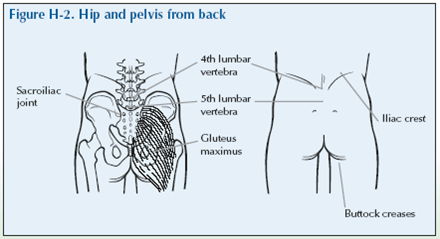
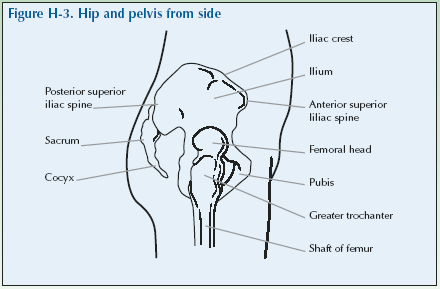
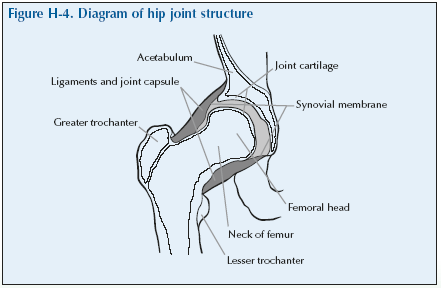
The hip is the main weight-bearing joint of the body, located deep under layers of powerful supporting muscles and ligaments. It is a ball and socket joint with the head of the femur forming the ball which inserts into the acetabulum of the pelvis.
Just distal to the head and neck of the femur on the upper portion of the femur is a bony process: the greater trochanter, a broad flat process on the lateral aspect. The trochanteric bursa overlies the greater trochanter.
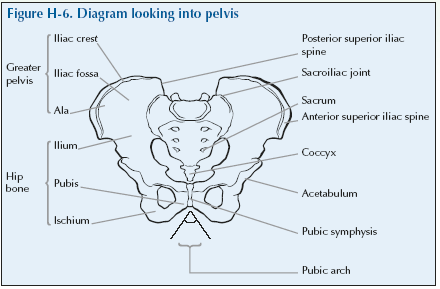
The pelvis and sacrum form an oval structure known as the pelvic girdle. The iliac crest is a ridge of bone formed by the upper, curved border of the pelvis. It can be palpated on the lateral aspect of the body just below the waist. The bony ridge ends in an anterior projection known as the anterior superior iliac spine (ASIS).
The pelvic girdle is joined to the fused part of the spine or sacrum at the sacroiliac joint.
Problems of the Buttock and Thigh
Pain in the hip may be coming from various structures – the lower back, pelvis, sacroiliac joints, soft tissues in the buttock including bursitis and also the hip joints.
Pain from the hip joint is usually felt in the groin or anterior or lateral thigh. Similar pain may also be caused by pain referred from the knee.
Buttock pain may originate from the hip but this is more usually due to problems in the lower back.
Pain in the outer thigh may arise from the trochanteric bursa or that region.
| Hip | Osteoarthritis
Rheumatoid arthritis Fracture |
| Bursitis | Trochanteric bursitis |
| Infection | Septic arthritis is rare |
| Sacroiliac joint | Mechanical |
| Inflammatory | Ankylosing spondylitis |
| Back problems | Pain in the buttock may be referred from the lumbar spine |
Osteoarthritis is one of the most common causes of hip pain in adults. A limp may develop with associated stiffness. In extreme cases a leg may become shortened and the hip adopts a fixed flexion and adduction deformity. Total hip replacement is effective in relieving pain in osteoarthritis.
Hip disorders:
- Often produce a limp.
- Cause a reduction in the distance that can be walked.
- Limit activities of daily living, such as getting in and out of the bath, or a car, putting on shoes and foot care.
Giving a History of Buttock and Thigh Pain
Invite the doctor to carry out a consultation by first asking you about your history related to the experience you have of your condition. This will then be followed by the physical examination.
The doctor should first ask you ‘What is the problem?’and you should give a short response describing your symptoms and their effect on your quality of life.
Develop a script based on your own experience. You may still have the symptoms or you may be describing an episode you have had as if it were still present.
Describe as fully as you can your own symptoms, including where in the buttocks, thighs or groin you feel/felt pain or discomfort. Say if you have any stiffness, swelling or other symptoms. Mention how the problem is having/had an impact on your daily life, your work, or your sleep.
Remember to describe how your condition affects/affected your quality of life. Consider self care (e.g. ability to wash, dress, toilet and feed), domestic care (e.g. ability to cook, clean, launder, shop), work (e.g. ability to stand, sit, type), leisure (e.g. ability to play sports, walk, go out for meals). Explain about the way it limits/limited your activities and restricts/restricted your participation in normal life.
Do not tell him everything spontaneously – just the important part. He will then need to ask further questions to fully characterise your problem. Develop a set of answers with your trainer to the following points. Prompt them if they omit important questions.
Pain is usually present and questions should establish:
- How the pain started and developed.
- The nature of the pain.
- The exact distribution of the pain.
- Whether the pain has increased or decreased over time.
- Whether it affects sleep.
- Whether anything exacerbates or relieves the pain.
Stiffness may be a symptom and questions should establish:
- If you are stiff at all?
- When it is worse?
- What improves it?
Swelling may be a symptom and questions should establish:
- If you have noticed any swelling and where.
- If it is always present.
- If it is painful or tender.
- If it is increasing.
They need to ask about the pattern of all the symptoms – where they started and if they have spread anywhere.
You may prompt the doctor (if you have not already told them) to make sure that they include the following information:
- Your age, occupation and hobbies.
- Your general health.
- Your past medical history.
- Whether you have any symptoms such as tingling, numbness or weakness in your legs.
- Whether there is any impairment of function and how this impacts on your daily activities and quality of life.
- Hip problems typically cause difficulty in walking, sitting down, rising from a seated position, putting on socks and shoes.
- Whether you have had previous treatment and if so whether it was successful.
The effect of any problem depends on your personal circumstances. The doctor needs to know about what you need to do in the home, at work, your leisure interests and your expectations.
You may have symptoms affecting other parts of your musculoskeletal system. You may prompt the doctor to ensure he has asked whether you have any other problems affecting your muscles, joints, neck or back.
You may go into further details about how your problem affects your life and the treatment you have received at the end of the session when discussing the findings.
Example of a Script
You should develop something like this, based on your own story. First you need to ask me:
“What is your problem?”
“I started getting pain in my groin 4 months ago when standing or walking for any length of time and it is beginning to stop me doing what I want to do.”
You should then respond to questions, guiding and prompting the doctor through the information as listed above.
directional terms you have learnt. You can use your knowledge of anatomy best when the doctor is feeling the joint and periarticular structures.
“I would now like to invite you to find out a little bit more about my problems, by role play, using me as your patient and examining me.”
Hip Examination Script
Describe the examination to the doctor using the anatomical and directional terms you have learnt. You can use your knowledge of anatomy best when the doctor is feeling the joint and periarticular structures.
“I would now like to invite you to find out a little bit more about my problems, by role play, using me as your patient and examining me.”
Look
Standing
Observe the patient walking to see if they have a normal gait. Look at them from the front and back when standing (or lying if they are unable to stand) for any asymmetry or muscle wasting.
What do you see?
Feel
Standing
With the patient standing if possible, palpate the buttocks for any tenderness to try and locate where the pain is.
With the patient standing if possible, feel for tenderness over the sacroiliac joints which may be located approximately 1” (2.5 cm)
laterally from the Dimples of Venus, or by drawing a finger from the ASIS back to the spine and then moving fingers laterally 1-2” (2.5 – 5cm).
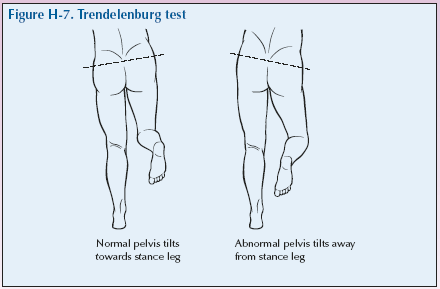
With the patient standing, place your hands palm down around the waist so that they are resting laterally on the pelvic brim. Then ask the patient to stand on one leg (their best hip) and then on the leg of their affected hip. Where there is a hip problem the pelvis may tilt and the unaffected (non-weight bearing) hip will dip below the horizontal because of weakness of the gluteus medius hip abductors. Normally the abductors keep the individual’s hips level. This is the Trendelenburg test.
Lying down
Now ask the patient to lie down on the examination couch, observe if they have any difficulty doing this. Palpate the pelvic rim and the greater trochanter for tenderness. This can be found approximately one hand’s width below the ASIS on the lateral aspect of the hips. This is usually the widest area of the hips when the patient is supine and you can recognise it as being the hard tissue in the lateral buttock. The trochanteric bursa overlies this structure. Palpate over both sides simultaneously.
What do you feel?
Move
Lying down
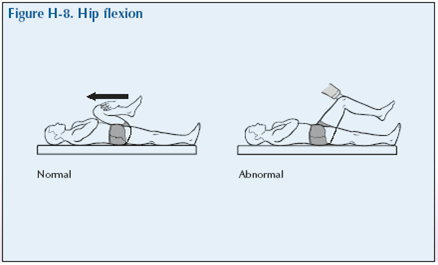
Flexion With the patient lying supine on their back, place one hand on the distal femur around the knee and put the other hand under the heel to give good support to the leg to allow the patient to relax the leg muscles. Now lift the leg flexing the hip and knee. It is important that the muscles are relaxed if you are testing range of movement. Use some pressure to flex the hip as far as it will go without hurting the patient. Always gradually increase pressure when moving a joint so you know if it is painful before pushing too hard.
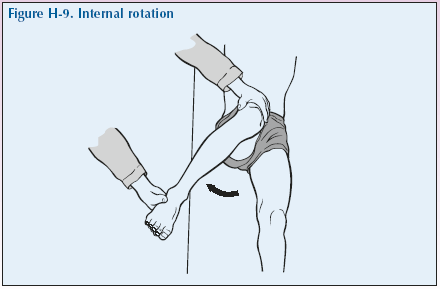
Internal rotation Keeping one hand on the knee and holding the heel with the other hand, lift and guide the leg until both the hip and knee are at 90°. Then rotate the lower leg outwards so that the thigh rotates inward (internally).
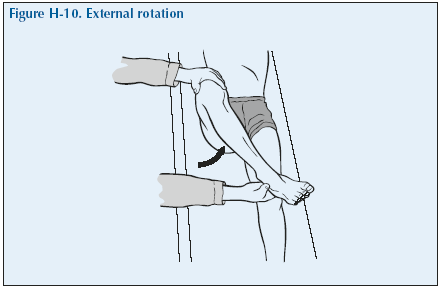
External rotation Now bring the lower leg back to neutral and then rotate it inwards so that the thigh rotates outward (externally).
As an aide memoire to help remember which way the hips is being rotated use the phrase “foot out/hip in, foot in/hip out”.
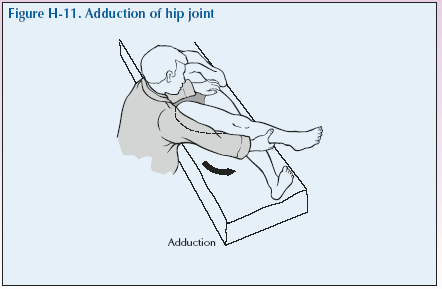
Adduction: Now, lower and extend the patient’s leg until it is straight but still elevated enough to clear the opposite foot. Place your hand over the opposite iliac crest. Then move the leg medially across the midline to assess the range of movement without movement of the pelvis.
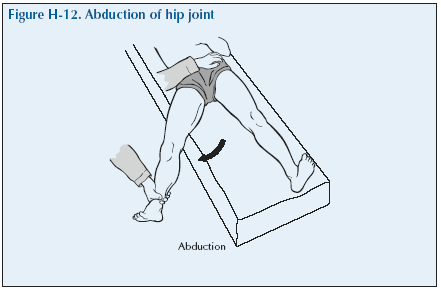
Abduction: Then, with the hand still over the opposite iliac crest, move the leg laterally until there is movement of the iliac crest (often a subtle “lifting”) which indicates the point of abduction.
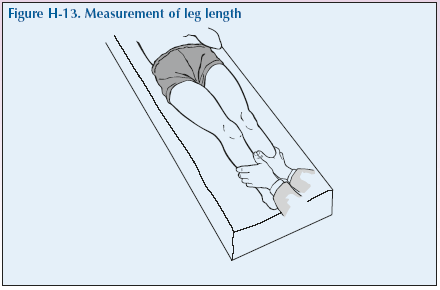
Leg measurement Assess whether the legs are the same length when the patient is lying with the pelvis straight and the legs outstretched by placing your hands around the ankles with your thumbs on each of the medial malleoli and feeling if they are side by side. You may want to measure both legs from the ASIS to the medial malleolus to more formally compare leg lengths.
What have you found?
Stress
Movement against resistance Test the quadriceps power with the patient lying with the leg extended. Place one hand proximal to the patella and feel the muscle and assess its strength when you ask them to lift the leg against your pressure.
Listen
Crepitus is uncommon but severe osteoarthritis can produce a “clonking” of the hip joint on movement.
Special tests
There are no special tests for use in a routine examination of the hip.
“We have now come to the end of this mock consultation. You should have learned quite a bit about my condition from taking my history and examining my joints, however, I would be happy to provide you with a bit more detail about the progress of my condition
and how it affects my life, if you would find this useful.”
[Please give a brief description of your condition:
- When and how it started.
- Physical and psychological affects on you.
- Treatments offered.
- How your condition progressed.
- How this affected your life: Home, education, work, leisure, ability to travel, relationships etc.]
“Does anyone have any further questions?”
“Thank you again for attending this session. I hope you have found it useful.”