Introduction
The elbow is a hinge joint connecting the two parts of the arm. Proper functioning of the elbow is necessary for full use of the hand, so elbow problems may sometimes appear as difficulty using the hand. The functional interplay of the shoulder, elbow and wrist means that examination of all three joints may be necessary. Cervical and shoulder pain may be referred to the elbow.
The forearm is in constant use and poor protection of the soft tissue around the elbow makes this joint particularly prone to problems with tendons or bursae. The elbow is not usually a primary site for arthritis, although it may be involved in inflammatory arthritides.
The elbow acts as a connector between the upper arm and forearm. There are two joints that make up the elbow.
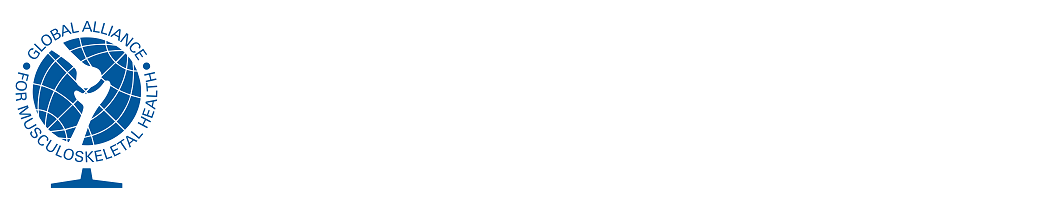
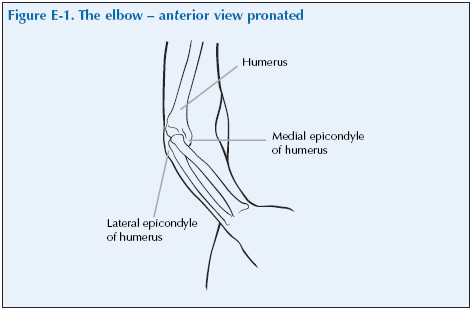
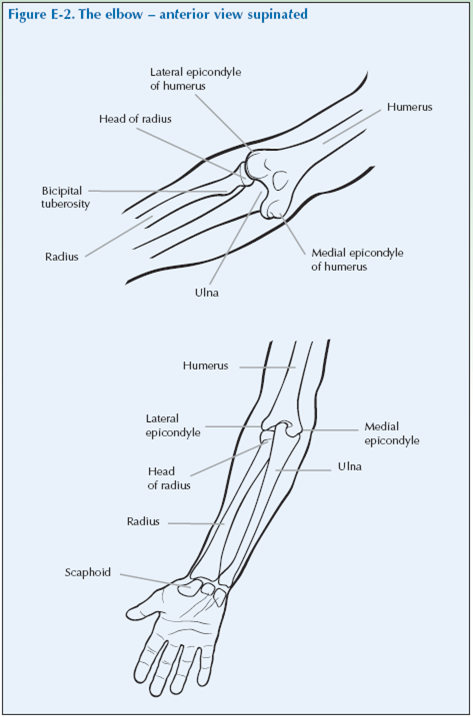
The humerus is the long bone of the upper arm which flares out at the distal end into the medial and lateral epicondyles that form the proximal part of the elbow joint. The radius and the ulnar are the bones of the forearm; the radius is on the thumb side and the ulnar on the little finger side. They form the distal part of the elbow joint. Flexion and extension occurs at the elbow joint. There is a joint between the proximal ends of the radius and ulna – the proximal radio-ulnar joint at which pronation and supination occurs. The proximal end of the ulnar is the olecranon process which is what we commonly call the elbow. The olecranon bursa lies over this process.
The large muscle in the back of the arm, the triceps, attaches to the point of the ulna (called the olecranon). When this muscle contracts, the elbow is straightened out. The biceps muscle in the front of the arm, when contracted, bends the elbow.
The forearm muscles which produce the movement of the hand at the wrist are attached to the epicondyles of the humerus. The extensor muscle which straighten (extend, dorsiflex) the hand at the wrist are attached to the lateral epicondyle and the flexor muscles, which bend (palmar flex) the hand at the wrist, to the medial epicondyle.
The ulnar nerve is one of the major nerves of the arm. It originates in the neck and runs down the inner side of the upper arm to behind the elbow. In the forearm it supplies the muscles with motor nerves (nerves that make the muscles move). Lower down it divides into branches that supply the skin of the palm and fourth and fifth fingers. As it passes in a groove over a prominence of the humerus at the back of the elbow it is close to the surface and therefore is vulnerable to knocks which can cause acute pain, numbness and a tingling sensation in the forearm and hand.
Problems of the elbow
Elbow problems usually present as complaints of pain, loss of movement, weakness, clicking or locking. Elbow pain may spread down the arm.
Soft tissue lesions are more common than joint diseases.
Periarticular causes
Lateral epicondylitis
‘Tennis elbow’ usually brought on by over or abnormal use of the elbow.
Medial epicondylitis
‘Golfer’s elbow’ usually brought on by over or abnormal use of the elbow.
Olecranon bursitis
This may relate to pressure, inflammatory arthritis (rheumatoid arthritis, gout) or infection.
Rheumatoid arthritis and other arthropathies
RA often affects the elbow. Other arthropathies such as psoriatic arthritis and ankylosing spondylitis can involve the elbow.
Crystal arthritis
Gout and pseudogout may cause elbow pain, affecting the joint or bursa.
Osteoarthrits
Osteoarthritis does not often affect the elbow. It may follow previous injury.
Infection
Infection is an uncommon but important cause. This should always be thought of by the doctor as early diagnosis and treatment is necessary.
Neck and shoulder problems
Neck and shoulder pain can radiate down the arm to the elbow.
Wrist problems
Occasionally people feel pain in the forearm up towards the elbow from wrist problems.
Tennis elbow is the most common problem affecting the common extensor origin at the lateral epicondyle. Elbow pain is exacerbated by gripping with the hands when the arm is extended – this is due to stress on the tendons. It is often caused by excessive activity involving the elbow, hand and wrist. This may relate to sport, hobbies or occupation. It can also occur spontaneously. Lesions of other soft tissue around the elbow are rare.
Neurological problems result in poorly localised pain or tingling in the hands and fingers.
Neurological pain may be caused by nerve entrapment.
Giving a history of elbow problems
Before commencing the physical examination you should give a summary of your elbow problem. It is important to describe restricted or painful movement and to describe the quality of the pain and when it is most severe.
The doctor should first ask you ‘What is the problem?’ and you should give a short response describing your symptoms and their effect on your quality of life.
Develop a script based on your own experience. You may still have the symptoms or you may be describing an episode you have had as if it were still present.
Describe as fully as you can your own symptoms, including where in the elbow you feel/felt pain or discomfort and whether you have/had any tingling in your arms and/or hands. Say if you have any stiffness, swelling or other symptoms. Mention how the problem is having an impact on your daily life, your work or your sleep.
Remember to describe how your condition affects/affected your quality of life using the framework covered in the earlier section of this manual. Consider self care (e.g. ability to wash, dress, toilet and feed), domestic care (e.g. ability to cook, clean, launder, shop), work (e.g. ability to stand, sit, type), leisure (e.g. ability to play sports, walk, go out for meals). Explain the way it limits/limited your activities and restricts/ restricted your participation in normal life.
Do not tell him everything spontaneously – just the important part. He will then need to ask further questions to fully characterise your problem. Develop a set of answers with your trainer to the following points. Prompt them if they omit important questions.
Pain is usually present and questions should establish:
- How the pain started and developed.
- The nature of the pain.
- The exact distribution of the pain.
- Whether the pain has increased or decreased over time.
- Whether it affects sleep.
- Whether anything exacerbates or relieves the pain. Stiffness may be a symptom and questions should establish:
- If you are stiff at all?
- When it is worse?
- What improves it?
Swelling may be a symptom and questions should establish:
- If you have noticed any swelling and where.
- If it is always present.
- If it is painful or tender.
- If it is increasing.
They need to ask about the pattern of all the symptoms – where they started and if they have spread anywhere.
You may prompt the doctor (if you have not already told them) to make sure that they include the following information:
- Your hand dominance.
- Your age, occupation and hobbies.
- Whether you have injured or strained your elbow, or recently done a lot of repetitive activities with the forearm and hand.
- Your past medical history.
- Whether you have any symptoms such as tingling, numbness or weakness in your arms/hands/fingers.
- Whether there is any impairment of function and how this impacts on your daily activities and quality of life.
– Elbow problems typically produce difficulties in reaching for items, carryin items, eating, some aspects of personal care such as washing and toileting and playing sports.
- Whether you have had previous treatment and if so whether it was successful.
The effect of any problem depends on your personal circumstances. The doctor needs to know about what you need to do in the home, at work, your leisure interests and your expectations.
You may have symptoms affecting other parts of your musculoskeletal system. You may prompt the doctor to ensure he has asked whether you have any other problems affecting your muscles, joints, neck or back.
You may go into further details about how your problem affects your life and the treatment you have received at the end of the session when discussing the findings.
Example of a Script
You should develop something like this, based on your own story. First you need to ask me
“What is your problem?”
“I started getting pain in my right elbow five years ago and it is now also limited in movement. This stops me gardening and also makes my job difficult.”
You should then respond to questions, guiding and prompting the doctor through the information as listed above.
Elbow Examination Script
Describe the examination to the doctor using the anatomical and directional terms you have learnt. You can use your knowledge of anatomy best when the doctor is feeling the joint and periarticular structures.
“I would now like to invite you to find out a little bit more about my problems, by role play, using me as your patient and examining me.”
Look
Inspect the joint for swelling, redness or tenderness.
With the arm in the extended and supinated position the joint should be inspected anteriorly for the carrying angle.
Look for any swellings.
Increased synovial fluid production or accumulation can be seen as a fullness in the lateral infracondylar recess. Pressure will obliterate the swelling in cases of effusion.
Hard bony swellings may be the result of previous fractures. Posteriorly, swelling of the elecranon bursa may be detected.
Rheumatoid arthritis may cause arthritic nodules which extend along the distal border of the ulna.
What do you see?
Feel
Feel for heat using the back of the hand all around the elbow joint.
Feel to locate the epicondyles and olecranon. They are easy to feel as they are close to the surface.
Palpate the elbow for tenderness, in particular over the medial and lateral epicondyles and olecranon.
Tenderness over the lateral epicondyle is typical of lateral epicondylitis.
Palpate the grove between the lateral epicondyle and olecranon for swelling – this is where the synovium bulges if there is inflammation of the joint. Feel with increasing pressure to see if it is tender.
Establish whether there is pain on movement.
Medially the ulnar nerve may be palpated between the olecranon and the medial epicondyle to detect thickening. Pressure on the nerve may produce tingling down the arm if it is already under some pressure.
What do you feel?
Move
The motions of the elbow are flexion, extension, pronation and supination.
Active Range of Motion (ROM)
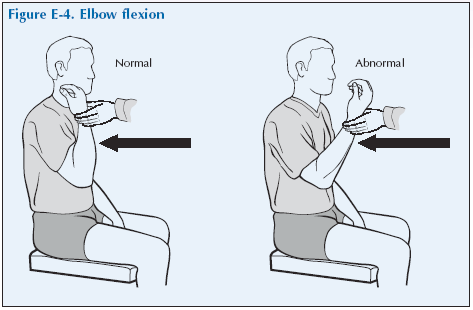
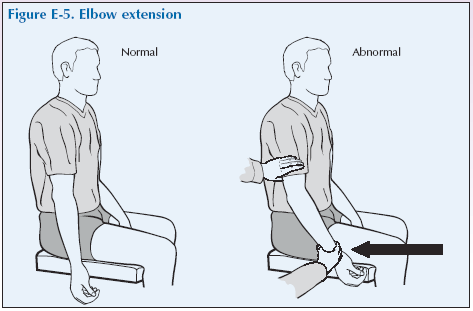
Ask the patient to fully flex and then extend their elbows (active range of movement) and use gentle force if it is limited to see if the range can be increased (passive range of movement). Note any loss of flexion or extension (fixed flexion deformity) and any hyperextension.
Ask the patient to pronate/supinate the forearm with the elbow flexed at 90°. (Hold out their hands palms downwards and rotate to palms upwards and back to palms downwards (see wrist section for a diagram) (active range of movement) and then use gentle force if it is limited to see if the range can be increased (passive range of movement).
Passive ROM
The elbow should then be assessed using gentle passive movement if active movement is limited. This will not give any extra information if there is full active range of all movements.
Flexion Gently move the forearm as close as possible to the upper arm and estimate the maximum angle of passive elbow flexion by eye.
Extension The upper limb is straightened at the elbow to achieve maximal elbow extension. When it is not possible to straighten the elbow completely, the maximum angle achieved subtracted from 180° is referred to as the angle of ‘fixed flexion’ of the elbow.
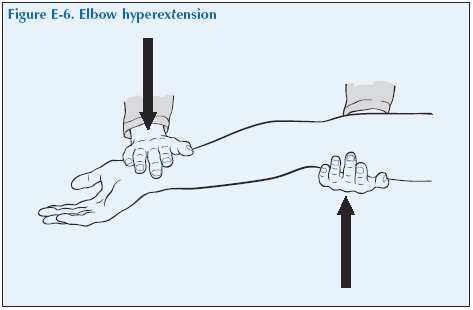
Where extension proceeds to beyond a straightening of the arm there is elbow hyperextension. More than 10° movement from the 180° position is considered to be a significant degree of hyperextension.
What have you found?
Stress
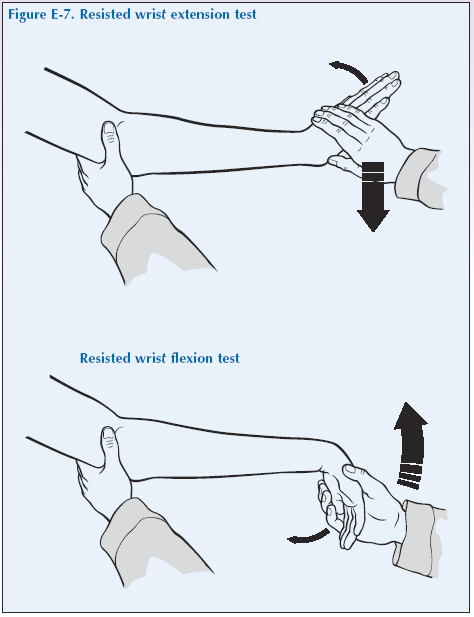
Resisted active wrist extension will produce tenderness and may cause the pain of lateral epicondylitis. Resisted active wrist flexion will produce tenderness and may cause pain of medial epicondylitis. This should be done with the elbow at 90° flexion and press with the thumb on the relevant epicondyle for tenderness.
Listen
Listen for crepitus, but it is uncommon.
Special tests
There are no special tests for use in a routine examination of the hip.
“We have now come to the end of this mock consultation. You should have learned quite a bit about my condition from taking my history and examining my joints, however, I would be happy to provide you with a bit more detail about the progress of my condition and how it affects my life, if you would find this useful.”
[Please give a brief description of your condition:
- When and how it started.
- Physical and psychological affects on you.
- Treatments offered.
- How your condition progressed.
- How this affected your life: Home, education, work, leisure, ability to travel, relationships etc.]
“Does anyone have any further questions?”
“Thank you again for attending this session. I hope you have found it useful.”