Before we continue to learn about the musculoskeletal system in detail we need to consider some background information about the types of musculoskeletal problems and conditions and about the terminology used during medical examinations.
Types of musculoskeletal problems and conditions
There are a surprisingly large number of conditions (over 200) that can affect the musculoskeletal system. A careful history and examination will allow the doctor to classify the condition into one of the following broad groups:
- Conditions affecting the joints. “Arthritis” is used to describe these conditions:
- Osteoarthritis.
- Inflammatory arthritis, such as rheumatoid arthritis or gout.
- Conditions affecting the spine:
- Neck pain.
- Back pain.
- Conditions affecting soft tissues:
- Bursitis.
- Tendonitis.
- Fibromyalgia.
- Conditions affecting the bones:
- Osteoporosis
Sometimes a person has pain affecting the musculoskeletal system and no physical cause can be found.
It is beyond the scope of the programme to consider all of the musculoskeletal conditions in detail, so we shall concentrate on the more common ones. It is important to remember that other conditions do exist and as a Patient Partner you may have one of these other conditions. Do not be worried by this; the ability to demonstrate your own joint function is what is crucially important to the programme. If you would like to learn more about musculoskeletal conditions, then there are some books and websites listed at the end of the manual that you may find helpful.
Osteoarthritis
(os-tee-oh-are-thry-tis)
Osteoarthritis (OA) affects about 15 people in 100, and after age 55 is more common in women than men.
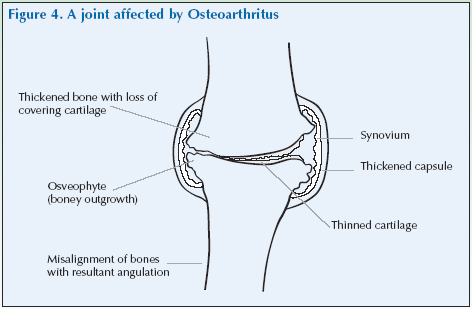
In OA there is a thinning, often progressing to complete loss, of the cartilage that covers the surface of the joint (Figure 4). It can also affect the underlying bone.
OA may arise without an apparent cause or may occur after damage to a joint from inflammation (which might be a result of infection), too much stress on the joint or traumatic injury. It can sometimes run in the family. OA of the hip and knee are more common in people who are overweight.
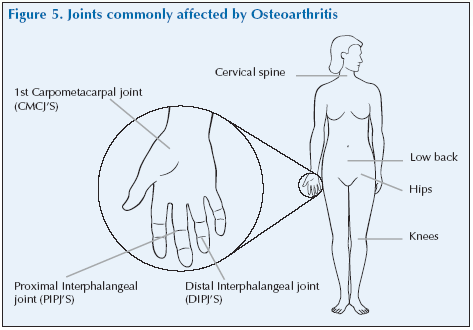
OA commonly affects load-bearing joints such as the spine, hips or knees and can also affect the finger joints; it may only affect one side of the body.
The most common symptom of OA is pain in the affected joint(s) after repetitive use. Joint pain is usually worse later in the day. There can be swelling, warmth and crepitus (creaking) of the affected joints.
Pain and stiffness of the joints can also occur after long periods of inactivity – for example, sitting watching television or in a car on a long journey.
In severe OA, complete loss of the cartilage cushion causes friction between bones, causing pain at rest or pain with limited motion.
Symptoms of OA vary greatly from patient to patient. Some patients can be debilitated by their symptoms. On the other hand, others may have remarkably few symptoms in spite of dramatic degeneration of the joints apparent on x-rays. Symptoms also can be intermittent. It is not unusual for patients with OA of the hands and knees to have years of pain-free intervals between symptoms.
Rheumatoid arthritis
(rew-ma-toyd are-thry-tis)
Rheumatoid arthritis (RA) occurs in one person in 100 and most commonly affects women between the ages of 40–50. It is an important cause of disability.
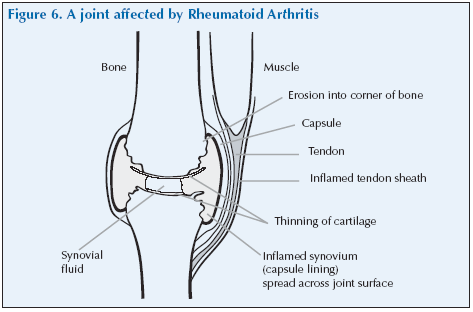
In RA there is inflammation of the lining of the joints which causes joint damage (Figure 6), which starts early and progresses slowly with time. It also has a major effect on what people can do, commonly causing people to have to give up their work. Modern treatments can slow down the progression of RA and have considerably improved the outcome over the past 10 years.
The causes of RA are unclear, but there is evidence of genetic predisposition to the disease.
RA is rare in young people; in men peak incidence is at age 60–70 years, in women it increases in incidence in the mid–20s to reach a fairly constant level at 45–75 years, being slightly greater at 65–75 years.
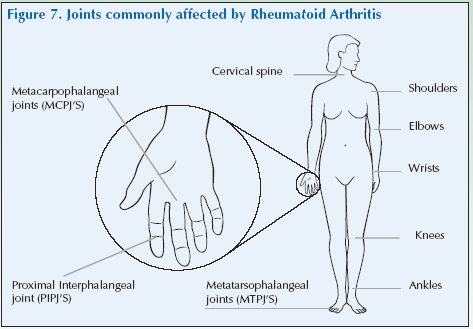
Typically, the condition most commonly affects the finger joints, knuckles and wrists, feet and ankles, progressing to the elbows, knees, shoulders and the hips and less commonly the cervical spine. RA generally follows a symmetrical pattern, meaning that if tne knee or hand is involved, the other one is also affected.
In addition, people with RA may have fatigue, and a general sense of not feeling well (malaise). Other features include lumps (rheumatoid nodules) under the skin in areas subject to pressure (e.g. back of elbows).
RA affects people differently. For a few people, it lasts only a few months or a year or two and goes away without causing any noticeable damage. Other people have mild or moderate forms of the disease, with periods of worsening symptoms, called flares, and periods in which they feel better, called remissions, and may result in gradually progressive problems.
Still others have a severe form of the disease that is active most of the time, lasts for many years or a lifetime, and leads to serious joint damage and disability. However, modern treatment can reduce inflammation and joint damage and improve the long-term outcome.
As shown in the diagrams above, there are important differences in the way OA and RA affect the hands and wrists. These differences are covered in detail in the hand and wrist section.
Terminology
In order to communicate effectively with doctors you will need to learn how to describe the body in medical terms. In the following sections you will encounter some fairly detailed anatomical descriptions of the joints which contain some unfamiliar and, at first sight, seemingly frightening and difficult words. Do not be daunted by these terms – they are not so difficult and, once mastered, you will be able to describe a joint with a degree of accuracy and economy of words that is simply not achievable using “everyday” language.
Directional terms
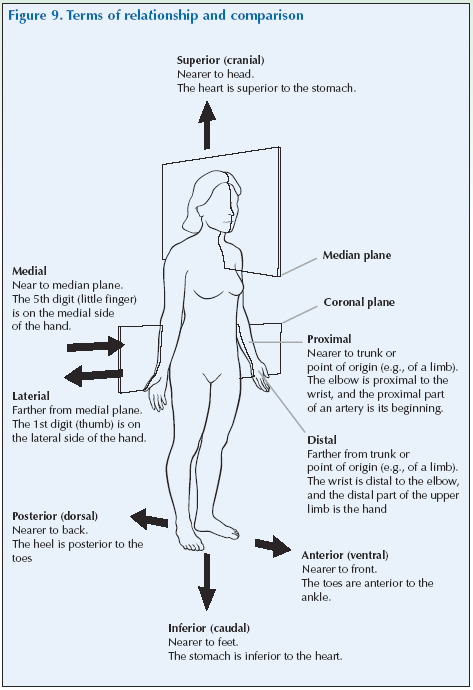
A number of directional terms are used to describe how the body is organised and how various structures are located in relation to each other.
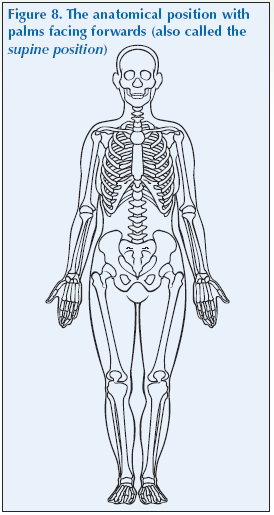
The starting point for these descriptions is the anatomical position. In this position the body is upright and facing forward, arms are outstretched with palms of the hands facing forwards and the thumbs facing away from the body. Unlike a theatrical stage, where the audience is looking at the actors and what is right to the audience is left to the actor, there is no ambiguity: right means the body’s right side and left the body’s left side wherever it is being viewed from.
If a person is lying down on his face, he is in the prone position with the palms of the hands facing down and thumbs out. Somebody lying on his back with the palms of the hands facing up and thumbs out is in the supine position.
The term superior means towards the upper portion of the body or limb; the term inferior means towards the lower portion of the body or limb. Also, a structure may be described as superior or inferior to another structure.
In anatomical terminology sometimes a shortened version of the word can be incorporated into other words. So when you come to the knee you will find a suprapatellar bursa above the patella (knee cap) and an infrapatella bursa below the patella.
Similarly the terms anterior and posterior refer to structures towards the front and towards the back respectively. Your knee cap is on the anterior aspect of your leg, your shoulder blade is on the posterior surface of the body. These terms are also used to describe position in relation to each other – for example, the nose is anterior to the ear.
The words to describe relative positions in the side-to-side direction are medial and lateral. Medial structures are close to an imaginary line down the middle of the body. Lateral structures are further away from the midline.
So when changes in the big toe joint occur that cause the bone of the foot (metatarsal) to move which produces a bulge inwards or towards the other foot and the big toe to point outwards or towards the other toes on the foot (commonly called a bunion), it is described medically as a medial displacement of the metatarsal and a lateral deviation of the phalanx (toe). (The medical name for bunion is hallux valgus).
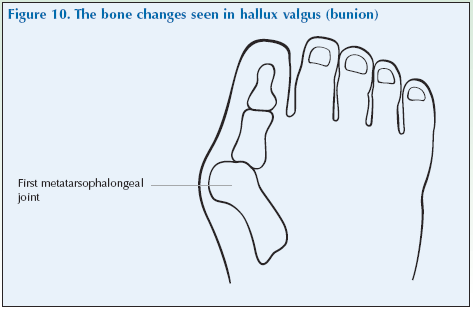
This is a classic example of the advantages of using seemingly complicated anatomical language. It took 36 words to clumsily describe the foot deformity in everyday language, but the anatomical description was unambiguous in just 12!
The last two useful terms are proximal and distal. Structures that are proximal are nearer the point of attachment, the centre of the body, or the point of reference. So an elbow is proximal to a wrist, a patch of skin on your thigh is proximal to one on your calf. Distal points are farthest from the point of attachment, the centre of the body or the point of reference. Your feet are distal to your knees.
**********************************************************************************************************************
Summary
| Superior | : | Toward the head |
| Inferior | : | Away from the head |
| Anterior | : | The front of the body or body part |
| Posterior | : | The back of the body or body part |
| Medial | : | Toward the midline that divides left and right |
| Lateral | : | To the side, away from the midline |
| Proximal | : | Closer to the torso |
| Distal | : | Farther away from the torso |
********************************************************************************************
Movements
**********************************************************************************************************************
Summary
| Extension | : | Increasing the angle of the joint |
| Flexion | : | Decreasing the angle of a joint |
| Elecation | : | Moving to a superior position |
| Abduction | : | Away from the body |
| Adduction | : | Towards the body |
| Rotation | : | Turning about the long axis of a bone |
| Supination | : | Rotating forearm laterally |
| Pronation | : | Rotating forearm medially |
**********************************************************************************************************************
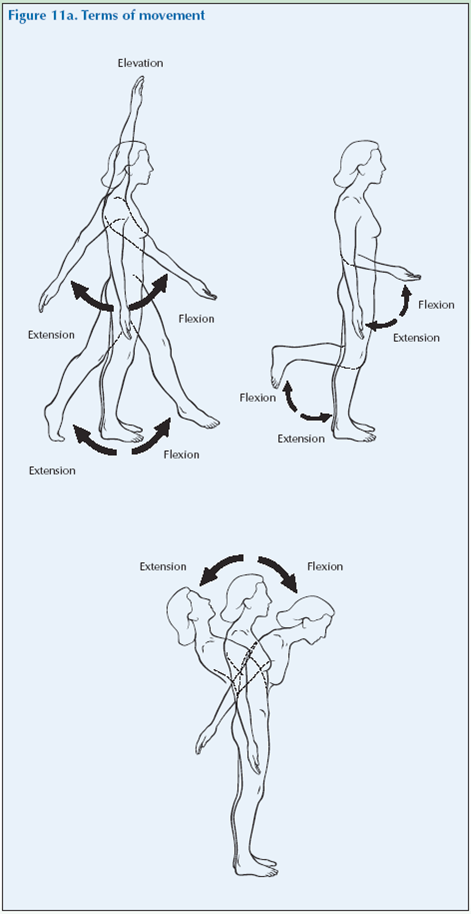
There are specific anatomical terms used to describe the movement of limbs or joints.
Straightening, or increasing the angle of a joint is called extension, while bending or decreasing the angle or making it smaller is flexion. So extension of the elbow will straighten the arm, and you will need to flex your knee to kneel down. (As an aide memoire remember extension is extending the length of your arm.)
Moving a limb to a superior position is elevation. So putting your hands above your head is elevating them.
Abduction refers to moving a limb away from the body or away from the midline. In abduction of the fingers it means spreading them apart – moving the other fingers away from the third or middle finger or moving the other toes away from the second toe.
Adduction is moving the limb in the opposite direction – towards the body or midline. Adduction of the digits means moving the fingers towards the third finger of the hand or the toes towards the second toe. (As an aide memoire, remember abducting someone is taking them away.)
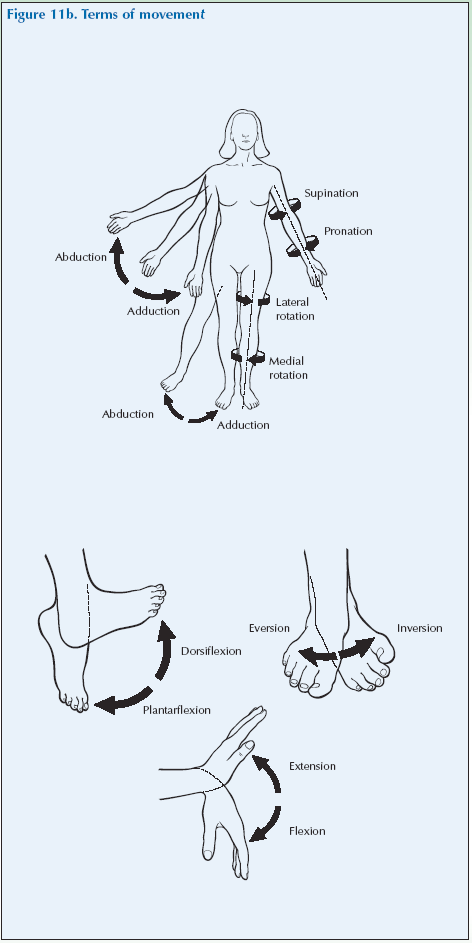
Rotation refers to turning or revolving a part of the body around its longitudinal axis, such as turning one’s head to the side.
Supination is rotating the forearm laterally to turn the thumb out and pronation is rotating the forearm medially to turn the thumb in. So if you hold you hand out in front of you with the back of your hand uppermost and thumb pointing inwards and then turn you hand over so the palm is uppermost and the thumb is pointing outwards you have performed a supination of your hand.
Introduction to the structure of the musculoskeletal system
The musculoskeletal system is composed of bones, joints, muscles and other connective tissues.
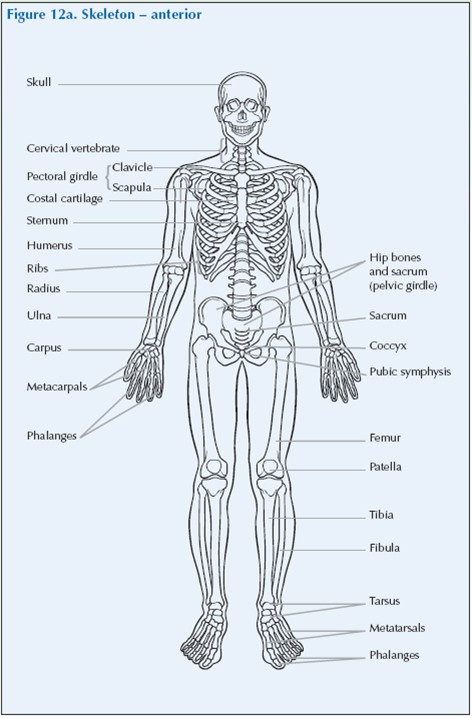
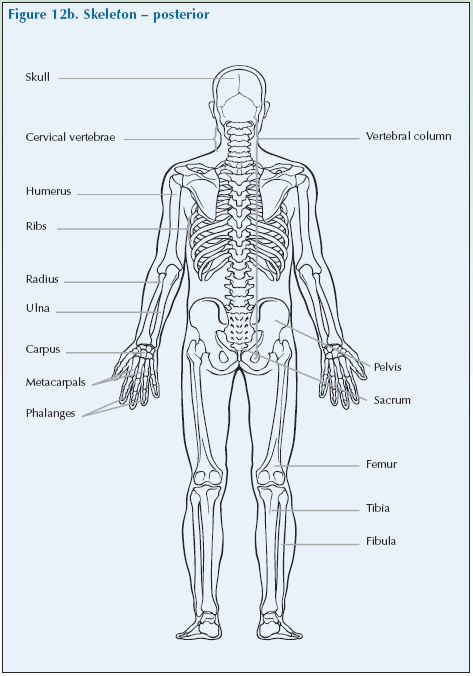
Bone
Bones form the skeleton which gives support for the body, protects vital structures and gives the mechanical basis for movement. The bones of the head, neck, trunk (ribs, vertebrae and sacrum) make up the axial skeleton. The limb bones make up the appendicular skeleton.
Cartilage
Cartilage is a resilient semi-rigid material that forms part of the skeleton where movement occurs. It may form the hinge of the joint itself. Alternatively, it may cover the ends of the bone in joints which move freely (synovial joints).
Joints
Joints are where two bones meet. Some joints have no movement, such as those between the bones of the skull, but movement is an important function of many joints.
There are three basic types of joint:
- a fibrous joint – relatively immoveable. These joints are firmly held together by a thin layer of strong connective tissue. There is virtually no movement between the bones. Fibrous joints include the sutures of the skull and the joint between teeth and their sockets.
- a cartilaginous joint – partly moveable. Cartilaginous joints are joints where the articular surfaces of the bones forming the joints are attached to each other by means of fibrocartilaginous discs which are soft and able to change shape (plastic or deformable) or ligaments which allow only a limited degree of movement. Examples are the cartilaginous joints between the vertebrae of the spine (the “discs” which so often become “slipped”), the cartilage in the symphysis which binds the pubic bones together at the front of the pelvic girdle and the cartilage in the joint between the sacrum and the hip bone.
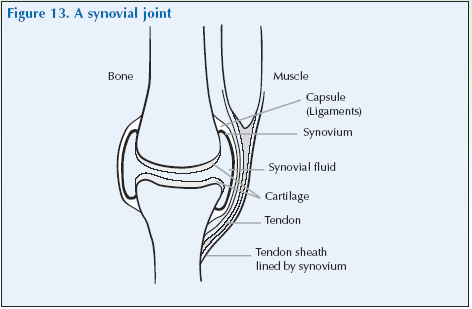
- a synovial joint – freely moveable. Synovial joints are where one surface slides freely over another and movement is positively encouraged – for this is the role of the synovial joint.
Periarticular structures
There are other structures around the joint. Joints are stabilised by ligaments, which are tough bands of white connective tissue that link two bones together at a joint. Ligaments are flexible but not elastic; they strengthen the joint and limit its movements to certain directions.
Tendons attach muscles to bones. The junction of the tendon and bone at the point of attachment is called the enthesis. Tendons are made of parallel bundles of collagen. Like ligaments, tendons are flexible and inelastic and assist in concentrating the pull of a muscle on a small area of bone. The flexor tendons in the ankle and wrist are surrounded by synovial membranes and fluid.
Movement of a joint is produced by contraction of muscles and the movement is transmitted via the tendons to the bones.
Bursae (singular bursa) are small sacs of fibrous tissue filled with synovial fluid. Bursae occur where parts move over one another and help to reduce friction and cushion joints. They are normally formed round joints and in places where ligaments and tendons pass over bones.
If the bones of a joint become displaced from their normal position such that there is a complete loss of contact of the joint surfaces, the joint is said to be dislocated. Luxation also means dislocation but this term is rarely used.
Subluxation refers to a partial dislocation of a joint, where the bones are still in contact but are not properly aligned.
Structure of a synovial joint
The ends of the bones forming a synovial joint are covered with a thin layer of cartilage and surrounded by a capsule which is lined with a synovial membrane that secretes synovial fluid to lubricate the joint. There are also several bursae which are fibrous sacs also lined with a synovial membrane and containing small amounts of synovial fluid. These sacs occur where parts move over each other, to reduce friction. They occur around joints and in places where tendons and ligaments pass over bones.